Antimicrobial Stewardship programs work tirelessly to change prescribing behavior amongst their providers. Sometimes it’s an uphill battle. We spoke with Pediatric ASP team lead, Dr. Nicole Le Saux, to get her insights on how she is able to change prescribing behavior by evolving her guidelines as part of a conversation with her providers.
Tell us about your role in Antimicrobial Stewardship
Dr. Le Saux: I am the medical lead for stewardship at my hospital. We are a relatively small hospital so do not have a full time pharmacist dedicated to this role. We reasoned that the easiest way to have a culture change of antibiotic use was to make it easier to have prescribers access our evidence based guidelines, both in hospital and out of hospital. I am not tech-savvy in the least. The Firstline app is great since it is so easy to change recommendations, add links to key articles and websites that I or the younger pharmacist on my team does in a flash. The app is used by even physicians that have never used their phone in this way before. I’ve used Firstline at our hospital since 2016 and it has changed my life making it easier for me to have conversations about our guidelines. Even when I get calls, I can have them download it and show them where my recommendations are coming from or where to get the information they are looking for.
How do you teach stewardship to your providers?
Dr. Le Saux: I like to think of our guidelines as evolving, and use them as a teaching tool. I ask people to download Firstline on their phones so that we can review guidelines together, and sometimes even use it to show patients that you need to have symptoms to get an antibiotic.
On the wards when we do handshake stewardship, if someone tells me they don’t understand our guideline on sinusitis, for example, we’ll go to that section in the Firstline app and I’ll find out what part they don’t understand. Then, with them, I’ll change the wording of the guideline to make it more understandable. I’ll go back to my desk, make the changes in the Firstline platform and it will be instantly updated and more clear to the user. The guidelines get better and better as we go on.
If someone asks me “What are your clinical criteria for pneumonia?” we’ll go right to that section in the app and review it together.
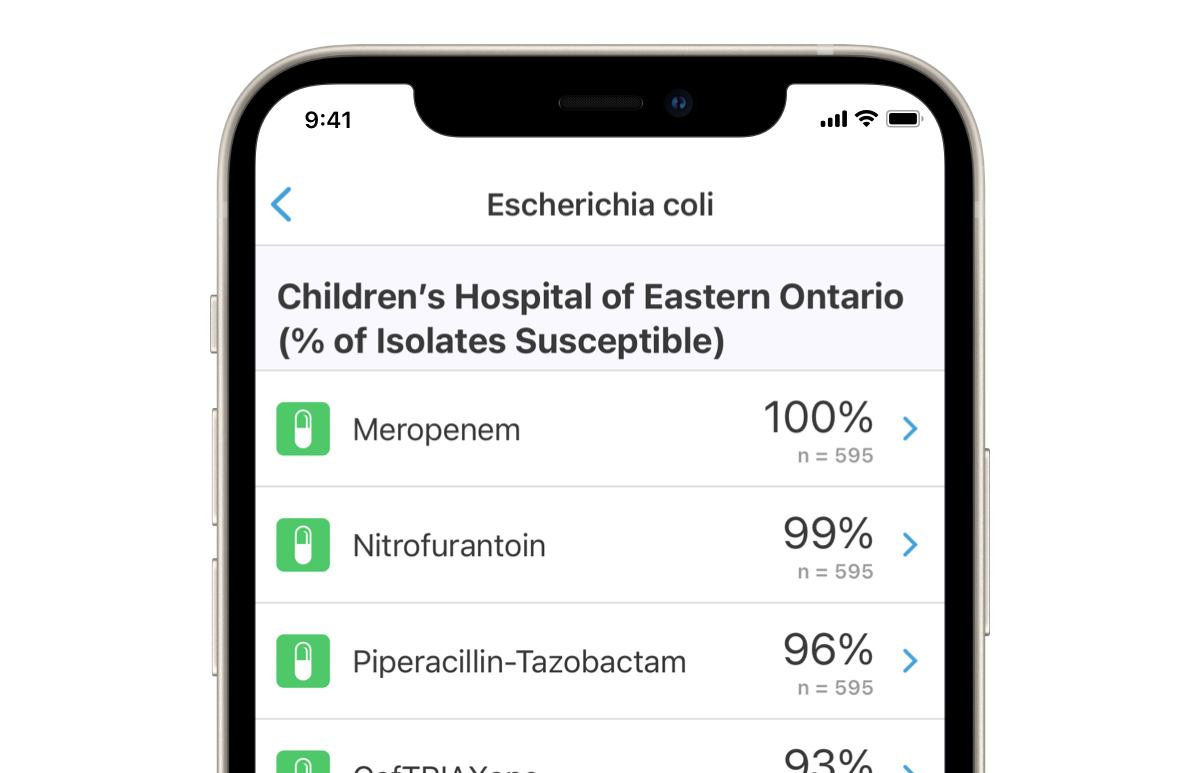
I’ll ask the residents to “open up your antibiogram and look at E. coli or pneumococcus and we can look at the antibiogram data together so they know what the local susceptibility patterns are. 99% of docs have no idea of the usefulness of the local antibiogram and after this … they get it! Respond and feedback. This is the best way to teach good stewardship.
Some things in the guidelines I take off of the app because I don’t want to give providers too much information that it becomes overwhelming. Sometimes, we add pictures for example with Lyme disease, to make sure it’s clear, and/or link to a reference on a website.
As a teaching institution, we find Firstline useful – people know that we are responsive because we are always changing and updating the app. We can import things that other institutions have created and link to them.
How can analytics help your stewardship program?
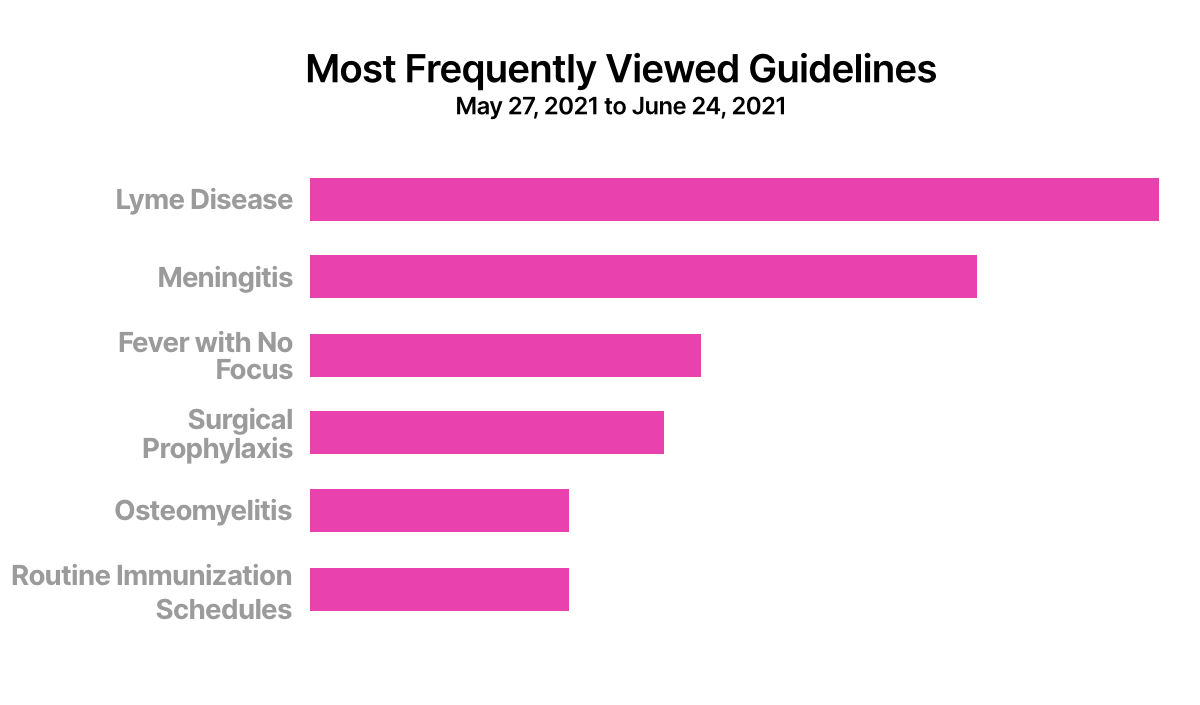
Dr. Le Saux: I look regularly at my active users in Firstline to see what people are looking at. Last week everyone looked at Lyme disease since it’s that time of year. I can tell who is using what information and respond accordingly.
How do you address Outpatient Stewardship using Firstline?
Dr. Le Saux: Emergency rooms and doctors offices located outside of the hospital with little formal training in antibiotics are prescribing often. It’s good to be able to easily remind them of what’s appropriate to prescribe. As well, there are now less errors in underdoing and inappropriate durations.
Family physicians in our community use it a lot and they ask me questions when I give talks. They also like the links to the routine immunization schedules.
How do you see prescribing behavior improve at your institution?
Dr. Le Saux: You get better prescribing because people go to the app to see what to prescribe and the duration. They are seeing updated information so are safe in changing or modifying practices.
What outcomes have you seen at your institution since you launched with Firstline?
Dr. Le Saux: I think people are more aware of diagnostic criteria and what to order as there is a small section at the top of each guideline on this. I now rarely see a duplicate spectrum of antibiotics which is better for patient care. I see that people are more comfortable with amoxicillin challenges since the app has the protocol. Any ED can now do this. In short, the Firstline app has become part of our culture of patient safety and good prescribing.
Check out Dr. Le Saux’s guidelines on Firstline
Biography
Dr. Nicole Le Saux MD FRCP(C) Pediatric Infectious Diseases/Antimicrobial Stewardship Professor and Pediatric Infectious Diseases Consultant at Children’s Hospital of Eastern Ontario (CHEO)
