Antimicrobial Stewardship programs are charged with the mission to improve patient outcomes. We recently spoke with Kyle Massey, Co-Director of the ASP at Northern Light Eastern Maine Medical Center, to learn more about how creating a culture for Antimicrobial Stewardship has resulted in significant reduction in DOTs. He shares his insights on how to motivate and educate providers, as well as how to continue to advance an already successful program.
Tell us about your role in Antimicrobial Stewardship.
Kyle Massey: I’m an infectious diseases (ID) pharmacist and, along with my ID physician partner, co-direct the Antimicrobial Stewardship Program at Northern Light Eastern Maine Medical Center. We’re a 400-bed non-profit community hospital and the flagship facility for a 10-hospital system located throughout the state of Maine. We have an amazing team staffed by a second ID pharmacist and an ID physician. In addition to the day-to-day stewardship activities, I provide leadership and direction for the ASP at EMMC and for our health system, ensure regulatory compliance, and lead quality improvement and research initiatives.
You recently received an accreditation as a Stewardship Center of Excellence from the Infectious Diseases Society of America. Congratulations! That designation recognizes healthcare facilities that implement and maintain highly effective Antimicrobial Stewardship Programs. Tell us, what are the key initiatives in your ASP?
Kyle Massey: Thank you, it has been quite a journey. Since I assumed this role in 2019, we’ve embarked on a broad array of initiatives largely focused on expanding and strengthening the infrastructure of our program to be in line with the CDC Core Elements. Prospective audit and feedback has been a fully staffed function at this hospital for over a decade so we spent the last 2 years working on EHR integration, developing antimicrobial use data models, and creating localized treatment guidelines.
Central to this expansion was the idea of creating a culture of antimicrobial stewardship at our institution. We know that antimicrobial stewardship is ubiquitous in practice, but often the recognition of that is limited. For example, a prescriber evaluating a susceptibility report and changing regimens, a nurse advocating for their patients to be moved to oral medications, a pharmacist identifying a serious drug-drug interaction or simply adjusting antimicrobial doses based on renal function – while these may be routine activities for staff, all of these are obviously antimicrobial stewardship functions.
To develop this culture of antimicrobial stewardship, we’ve sought to create ownership by fostering recognition and appreciation of these activities as practicing antimicrobial stewardship; then encircle our hospital staff with the resources, nudges, and support necessary to optimize those decisions.
What specific outcomes have you seen to achieve this designation?
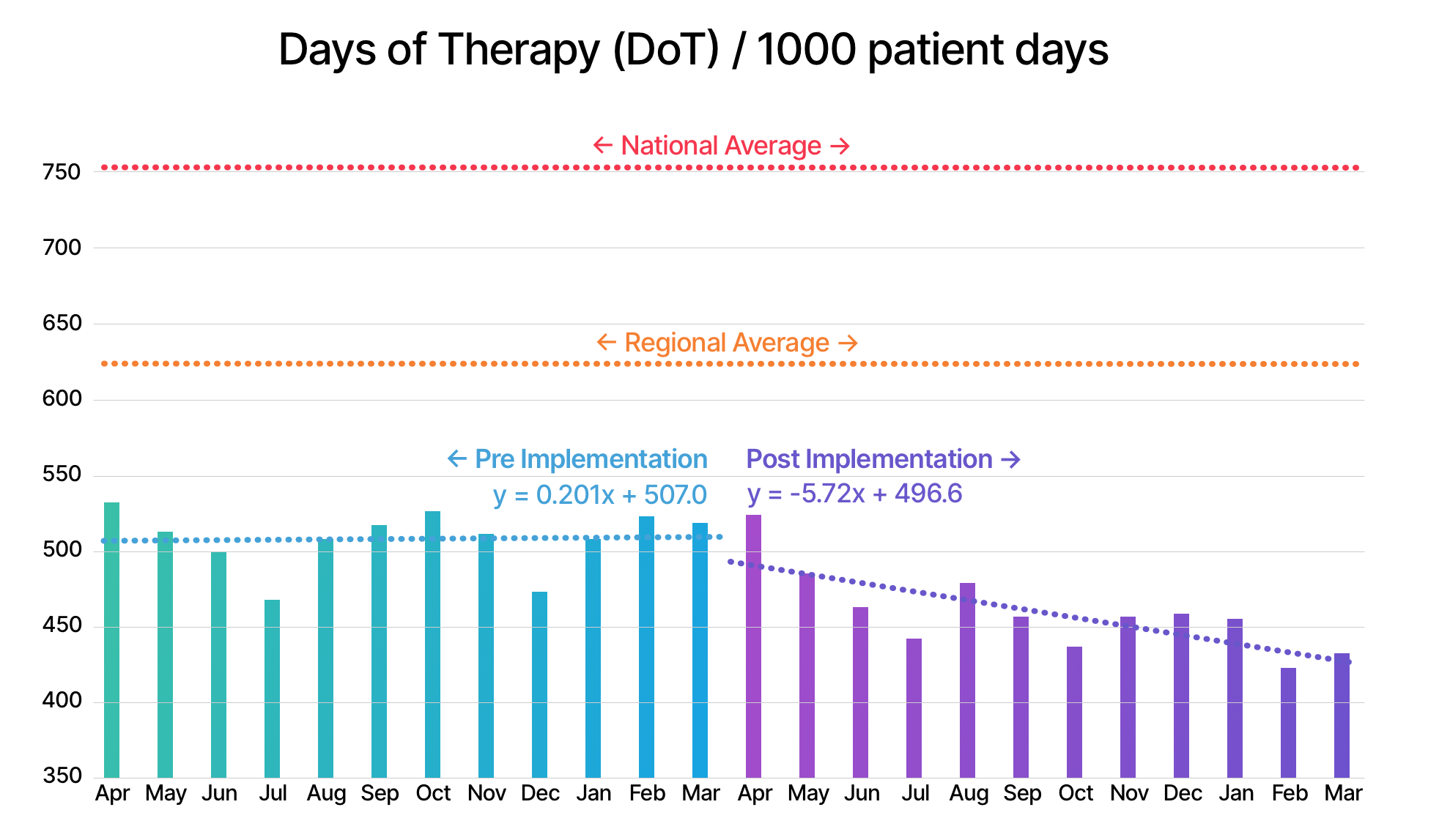
Kyle Massey: The full suite of our stewardship infrastructure, including our localized guidelines, launched in the summer of 2020. Since that time, we’ve seen a 10-15% reduction in overall antimicrobial use (days of therapy per 1,000 patient days) and use of targeted antimicrobials. Our mobile guidelines now have 170-200 active monthly users which represents a significant portion of our overall clinical staff. Of course, there’s a saying in advertising “I know half of my advertising works, I just don’t know which half”. The same applies here and we continue to evaluate individual aspects of our program for effectiveness and efficiency. But we have been impressed by the uptake of the mobile app and the user feedback we’ve received to date.
What role do you think Firstline has played in building a culture of antimicrobial stewardship at Northern Light Eastern Maine?
Kyle Massey: Unlike Field of Dreams, just because we build it does not mean they’ll come. There are many clinical decision resources and knowledge bases available for infectious diseases and antibiotics (e.g. Up-to-Date, Lexicomp, Hopkins guide, Sanford Guide) and often these are positioned directly in our EHR’s.
Unfortunately, these resources do not always account for local nuances such as formulary, local antibiograms, or the demographics of your catchment area. Firstline plays an important role here by allowing us to meet our prescribers, pharmacists, nurses, and other clinical staff where they are. Specifically, by providing a knowledge base platform that can be accessed online and at the bedside via mobile phone.
This has allowed us to place our guidelines in preferential positions over alternatives, easily share links to specific guidance, and – via mobile push notifications – quickly communicate changing guidelines and new developments. The latter has been particularly valuable during the COVID-19 pandemic.
What insights and tips can you share with other ASPs in our community on building a culture of antimicrobial stewardship?
Kyle Massey: I think marketing and branding is often an undervalued tool within the stewardship repertoire. Branding and name recognition can keep your program top-of-mind to staff and leadership. For example, rather than have our program identified as a Department of Pharmacy or Infectious Diseases initiative, we try to clearly delineate the resources and work of the Program from the groups that support it. Something like ‘Antimicrobial Stewardship, brought to you by…..”.
We even take painstaking care to create clear, consistent definitions around things like our guidelines (‘The Antimicrobial Treatment Guide’), ‘Antimicrobial Stewardship Program (ASP)’, ‘Antimicrobial Stewardship (AMS)’, and ‘Antimicrobial Stewardship Team (AST)’. Finally, we network and integrate our expertise into pathways around the hospital – for example, any time an order set that includes antimicrobials is requested or updated, the ‘Antimicrobial Stewardship Team’ is added as part of the review and approval process.
Every institution operates differently, and approaches should be tailored to each hospital or system. Ultimately, if we don’t position ourselves as the primary authority for antimicrobial use, and create a culture that values that expertise, it becomes very challenging to ensure a consistent seat at the table.
What’s next for your ASP to move the needle forward in continuing to improve prescribing behavior? How can Firstline help?
Kyle Massey: One of our big initiatives this year is expanding antimicrobial stewardship into the outpatient setting. We participated in the AHRQ Ambulatory Stewardship project last year and used that as a springboard to acquire IT support to build a broader data model around antimicrobial prescribing for acute respiratory tract infections in our outpatient clinics. We’re combining direct feedback from this data with an array of guidance for these conditions housed within Firstline.
One of our long-range goals, which I think is super interesting and exciting, is to engage our outpatient pharmacists to take a greater clinical role in affecting antibiotic decision making. We’re exploring ways to improve sharing of the indications associated with an antibiotic prescription from the clinic to the pharmacy and we plan to utilize Firstline as a platform to easily share guidance to the pharmacists to inform feedback based on that indication.
Check out Northern Light Eastern Maine’s guidelines in Firstline
Join Kyle and other ASP leads in the new Firstline Community - a free platform connecting all infectious disease specialists, to share guidelines, learn from each other and spread trusted knowledge.
