Working at Firstline, we see several hospital antimicrobial stewardship teams incorporate Penicillin Allergy De-Labeling strategies into their local guidelines to help limit unnecessary use of broad spectrum antibiotics. We recently interviewed Dr. Tiffany Wong and Dr. Chelsea Elwood, both of BC Women’s and Children’s Hospital in Vancouver, Canada to gain insights on this stewardship challenge and learn more about how they are using Firstline as an intervention tool to address it.
Tell us about Penicillin Allergy de-labeling - what is it and why is it important to treatment of infectious diseases?
Dr. Wong: Penicillin allergy de-labeling is a proactive approach to interrogating penicillin allergy labels. Taking an accurate medical history combined with validated penicillin skin test results and/or oral challenge of penicillin can identify patients who can safely receive penicillin and other β-lactam antibiotics.
It is important because 10% of patients in North American studies report having a penicillin allergy label; however, upon full evaluation by an allergist 90% of these people do not have a true penicillin allergy. There is robust evidence to indicate that penicillin allergy labels are associated with less effective, more expensive therapy with increased risk of adverse effects and antimicrobial resistance when alternative medications are used.
What has been the problem or challenge presented by penicillin allergy labeling overall and specifically at BC Women’s & Children’s? What are the costs associated with this problem at BC Women’s & Children’s?
Dr. Wong: Traditionally, penicillin allergy assessments were done by allergists. However, there are relatively few allergists and the number of people requiring assessments far exceeds the available capacity – leading to long wait times when patients are referred. In addition, the long wait times have deterred physicians from having patients referred to begin with. All of these patients end up receiving less desired, alternate therapy.
Dr. Elwood: For pregnant women specifically the long wait list means women will deliver prior to being assessed. About 50% of women will require an antibiotic in labour the most common of which is a beta lactation antibiotic. For example this is used to prevent group B streptococcus infection in babies, surgical site infection after cesarean section and the management of fever in labour. If a woman has an allergy to penicillin this changes what we can prescribe. The best approach is to have them evaluated before they deliver.
Multi-disciplinary penicillin de-labeling programs and clinics at BCWH have been very important in providing a proactive, structured approach to this problem but even these programs do not have the capacity to assess everyone with penicillin allergy labels.
How does penicillin allergy labeling impact antimicrobial stewardship?
Dr. Wong: We know that having a penicillin allergy changes prescriptions to broader spectrum antibiotics and alternatives which may not be as effective. In the long term this creates antimicrobial resistance. By clarifying someone’s allergy status, given that most are not allergic, we can then prescribe more narrow spectrum targeted antibiotics.
At BCWH our Penicillin allergy testing clinic has shown a direct benefit for prescribing in labour. All the women who have come through our clinic and have tested negative have gone on to receive Penicillin safely when it was required. For those women who were not tested, almost every one received a broader spectrum alternative. This has shown that clarifying allergy status prior to delivery has a direct impact on AMS.
Tell us about the tool you’ve created within Firstline to address this challenge.
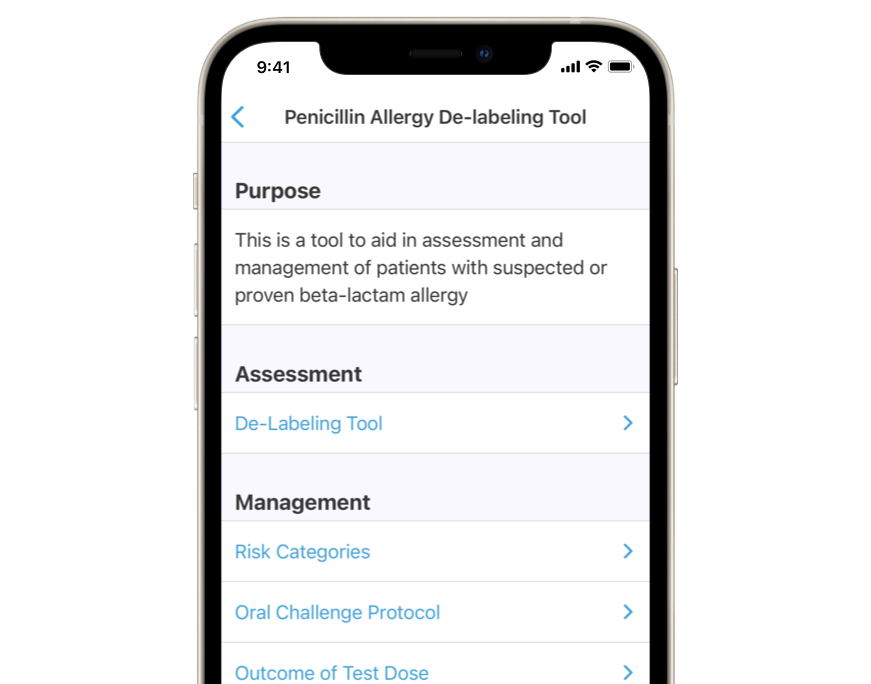
Dr. Wong: If most patients are not truly allergic to penicillin, then most health care providers are able to identify low risk patients for de-labeling. The challenge for busy practitioners is lack of confidence and knowledge in assessing risk of penicillin allergy. We have created a point-of-care risk assessment tool designed to guide busy practitioners through a penicillin allergy assessment. The assessment tool is based on the current published guideline and can be used for patients of all ages, including pregnant patients. The mobile application will allow real-time history taking and electronic answer submission. Back-end coding for the clinical algorithm enables a level of risk to be identified based on the answers provided by the clinician. The mobile tool will be available on Firstline via app or web for any who wants to use it. I was granted Medical and Allied Staff Association (MASES) facility engagement funding to develop an analytics dashboard with Firstline. Usage of the mobile tool will be monitored, along with satisfaction surveys to identify gaps in knowledge and to continually improve the mobile app. We aim to go live with this tool in May 2021.
Why did you choose Firstline to help build this tool?
Dr. Wong: Firstline is already being used as a tool for antimicrobial stewardship resources within BCWH. Penicillin allergy resources were already included in the application and the Firstline staff are familiar with this area of medicine. It was a natural fit to work with Firstline. Because Firstline already has a partnership with BCWH, it also makes sense from a sustainability perspective to house the algorithm and analytics dashboard within the app.
What are the benefits of this new tool?
Dr. Wong: There are several benefits of using Firstline for penicillin allergy de-labeling:
- Accessible to any healthcare provider at no cost Real-time guidance through risk assessment with point of care answer entry and immediate risk assessment and management recommendations provided
- Eliminates the need to look up practice guidelines and working through flat-form algorithms, although this option remains available within Firstline
What is your hypothesis for the outcomes this tool will generate? How will you measure the outcomes?
Dr. Wong: We aim to disseminate this tool widely across British Columbia, within hospital and community settings. We are fortunate to have been granted MASES Facility Engagement funding for Firstline to develop an analytics dashboard that will help analyze usage of the assessment tool. We will be able to determine type of practitioner, location of practice, percentage of patients reaching various risk categories, for example. We will also be including a satisfaction survey and provide opportunity for user feedback. The data we collect will inform improvements to the mobile tool, and help us target further healthcare provider education. It is a difficult thing to measure, but our overall goal is to reduce new and old erroneous labels of penicillin allergy in patients.
For more information on the Penicillin Allergy de-labelling program at BC Women’s and Children’s Hospital visit DropTheLabel.
Biographies:
Tiffany Wong MD, FRCPC Medical Lead, BCWH Allergy Clinic Clinical Assistant Professor, University of British Columbia, Department of Pediatrics Division of Allergy and Immunology, BC Children’s Hospital Hudson Scholar 2020/22
Chelsea Elwood B.M.ScH, M.Sc, MD, FRCSC Reproductive Infectious Diseases Specialist, Department of Obstetrics and Gynecology, University of British Columbia